Diverticular Disease and Diverticulitis
Diverticular disease is extremely common, especially as we age, and can cause ongoing gut discomfort that disrupts daily life. As a specialist dietitian service, we help people reduce pain, settle flare-ups, improve bowel regularity and feel confident with food again.
This page explains what diverticular disease is, why symptoms develop, what to eat during and after a flare, and how personalised nutrition can support long-term gut health.
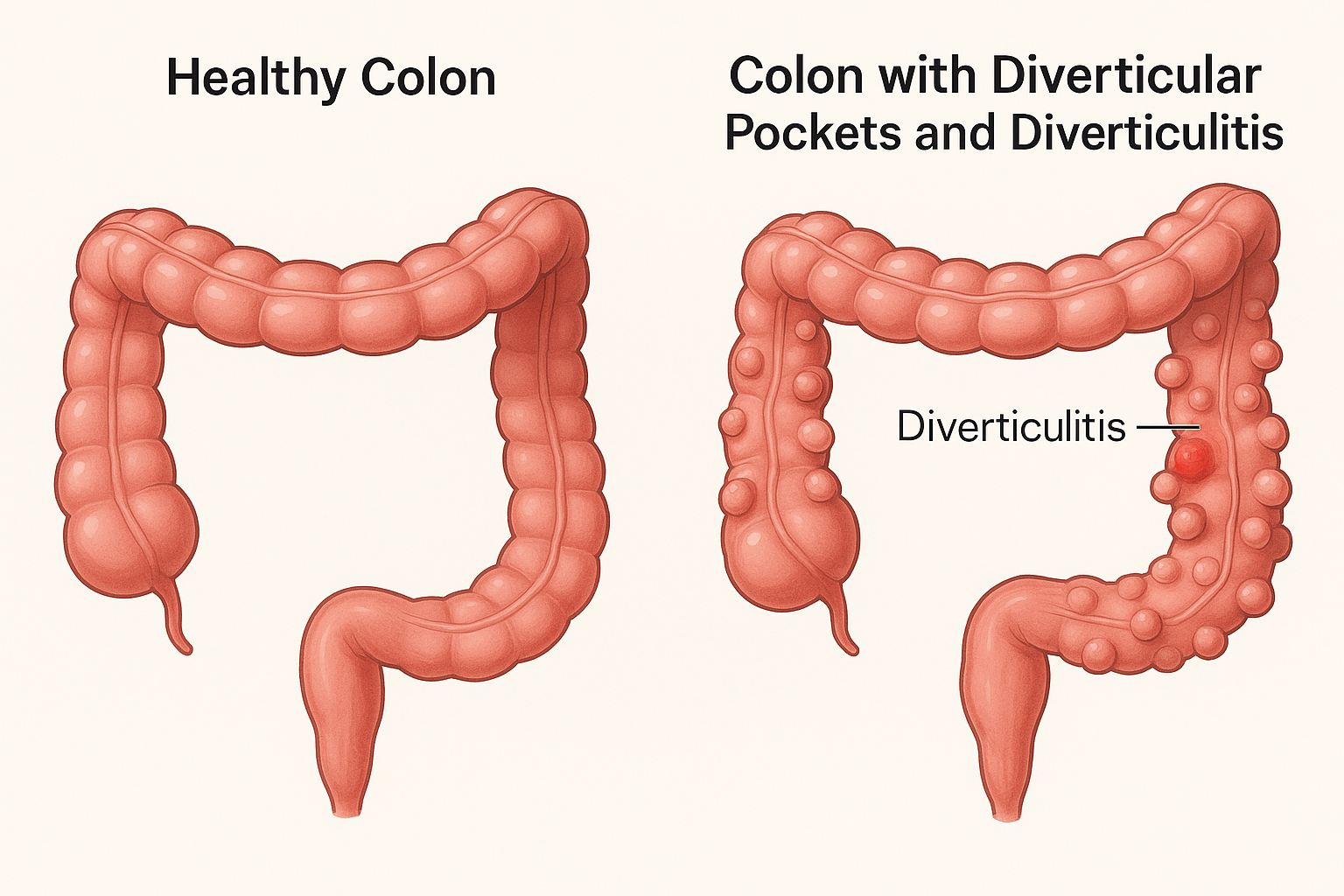
What Is Diverticular Disease?
Diverticular disease occurs when small pouches form in the wall of the large bowel. These pouches are known as diverticula.
Many people have diverticula without symptoms. Problems arise when the bowel becomes irritated, inflamed, or when the pockets trap food or stool.
Diverticulitis is the more acute stage when inflammation becomes significant enough to cause pain, fever or infection.
Common Symptoms
Symptoms vary from mild discomfort to acute episodes of diverticulitis. You may experience:
• Lower abdominal pain, often on the left side
• Bloating or swelling
• Burping or wind
• Constipation or irregular bowel habits
• Diarrhoea
• Nausea
• Cramping after meals
• Fatigue during flare-ups
Symptoms often overlap with IBS and other gut conditions, so a clear dietary approach is essential.
Why Symptoms Occur
Diverticular symptoms can be triggered by:
• Increased pressure inside the bowel
• Low fibre intake over time
• Poor gut motility
• Constipation and straining
• Food getting trapped in pockets
• Altered gut bacteria
• Stress or illness
• Medication changes
Understanding your personal triggers is a key part of preventing future discomfort.
Diet During a Flare-Up of Diverticulitis
A flare-up requires a different dietary approach than day-to-day management.
The goal during a flare is to reduce bowel workload and allow inflammation to settle.
A dietitian-guided flare diet may involve:
• Low residue or low fibre foods
• Softer textures that reduce irritation
• Gentle hydration strategies
• Avoiding tough skins, seeds, and fibrous vegetables temporarily
• Small, frequent meals if nausea or pain is present
This phase is temporary and should be followed by gradual reintroduction under guidance.
What to Eat for Recovery
Once pain settles and inflammation improves, the focus moves to rebuilding gut comfort and preventing further flare-ups.
Recovery eating often includes:
• Easily digested fruits and vegetables
• Gradual reintroduction of fibre
• Cooked rather than raw produce to start
• Adequate fluids
• Foods that support gut bacteria balance
• Spacing meals to avoid large bowel pressure
This is the stage where personalised nutrition is most powerful.
Long-Term Management for Diverticular Disease
Long-term dietary changes help reduce pressure in the bowel, improve stool consistency, and keep the diverticula from becoming irritated.
Supportive strategies include:
• Increasing fibre gradually to a comfortable level
• Including wholegrains, oats, vegetables and pulses
• Ensuring regular daily hydration
• Eating at consistent times
• Staying active to support gut motility
• Reducing overly processed foods
• Identifying your personal trigger foods
Every person’s tolerance is different, which is why a personalised plan works best.
Foods That May Trigger Symptoms
Some foods can increase gut pressure or worsen symptoms for certain individuals.
These may include:
• Tough skins or pips
• Large portions of red or processed meat
• Very high-fat meals
• Spicy foods
• Excess caffeine
• Alcohol
• Low-fibre patterns over long periods
This does not mean they must all be avoided; instead, they should be tested with care under professional supervision.
How Dietitian Support Helps
Many people feel unsure what to eat after a diverticulitis episode or ongoing discomfort. Individualised support can help you:
• Prevent flare-ups
• Reduce daily pain and bloating
• Improve regularity without triggering symptoms
• Rebuild confidence with food
• Resolve overlapping issues such as reflux, IBS, nausea or fatigue
• Understand fibre correctly rather than fear it
• Support your gut bacteria naturally
We use a structured approach that blends clinical experience, gut physiology, and practical food planning.
Your Personalised Diverticular Diet Plan
At 121 Dietitian we assess your symptoms, medical history, lifestyle, food preferences, and potential nutrient gaps.
Your plan may include:
• A phased dietary structure
• Flare-up protocol
• Recovery protocol
• Long-term fibre strategy
• Guidance on safe food reintroductions
• Supplement review if appropriate
• Strategies to prevent constipation
• Gut-friendly meal ideas
You receive ongoing support to ensure changes feel achievable and enjoyable.
When to Seek Medical Review
Always speak to your GP if you experience:
• Severe abdominal pain
• Fever
• Persistent vomiting
• Blood in stool
• Worsening symptoms over several days
• Recurrent flare-ups
• Unintentional weight loss
Diet and medical care work best together for managing diverticular disease.
Book Help for Diverticular Disease
If you are living with ongoing gut discomfort or recovering from diverticulitis, specialist support can make a significant difference.
We help you rebuild comfort, reduce inflammation, and create a diet that truly works for your body.

